Note: This post was originally published in 2017. Now that it’s 2020, we decided to give it an update. The core information remains the same.
Social service agencies across the world have voluntarily risen to the challenge of achieving accreditation. Whether their original goal was to focus on administrative functions or service delivery quality, the accreditation process (particularly with a whole-organization accreditation approach) provides these agencies with a blueprint to refine practices simultaneously across every area of the organization. The performance of these agencies has caught the eye of oversight entities and consumers alike, prompting accreditation to be used has a regulatory tool through mandates.
The word ‘mandate’, particularly in a government context, is notorious for creating concern across service providing agencies, often because of the cost associated with those requirements. COA believes all mandates function best when paired with the funding required to meet those mandates. We encourage all regulatory entities to consider the financial impact of any imposed mandate, as it can make or break the success of these initiatives.
Though the financial concerns of these agencies are absolutely valid, we can’t ignore the positives that can come with an accreditation requirement. Through accreditation, agencies are given a path to meet a base-level of quality across administrative and service delivery functions. Accreditation sets clear service expectations for service recipients and the taxpayers that fund these programs alike. It also fosters a culture of continuous improvement that can ensure the sustainability of an agency’s services. We cannot ignore the importance of these tenets in growing and maintaining a strong social service system that meets the needs of our communities.
To hopefully make this all a little easier on your organization, we’ve creating this guide to support your agency in navigating a mandate. Our goal is to help you gather important details, understand what is required, determine milestones, and know how to compare and contrast accreditors.
Note: Our best advice is don’t delay! Expect that it will take up to six months to determine an accreditor and then 12-18 months to pursue and achieve accreditation.
Questions for the entity that mandated your accreditation
What accrediting bodies are accepted?
Usually a mandate will include a list of accepted accreditors. If this isn’t included, reach out to the payer to find out what accreditors are accepted. If your preferred accrediting body isn’t recognized, we encourage you to reach out to that accrediting body and let them know. We can only speak for COA, but we are always willing to work with you and regulating entities to have COA accreditation be accepted under a mandate.
What service(s) is/are mandated?
Does the mandate apply to one service? Many services? The entire organization? Is there a document that crosswalks which services are mandated and what standards need to be applied by the accreditors? COA Accreditation Coordinators often know which service standard assignments are required for a mandate, but we always think it’s best for you yourself reach out to your regulatory entity to determine what is exactly required for your agency and the services you are providing.
What is due and when?
Mandates often come with specific timelines and may even have multiple milestone requirements. In these instances, regulating entities will designate a deadline for achievement of accreditation. To ensure organizations are on track to meet a deadline, regulating entities will designate milestone deadlines on the way to an accreditation award – a date by which organizations must engage with an accreditor, a date by which organizations must have their Site Visit, and then a date by which an award must be received.
What type of accreditation award is needed?
It’s important to clarify what type of accreditation award is due and when. Some accreditors offer provisional or temporary accreditation. Accreditors and regulatory entities will work with your organization to determine the type of accreditation award that is required under your mandate.
Evaluating accreditors — features to consider
Once you know which of your programs needs to be accredited, by when, and by whom, reach out to all the approved accreditors and get an understanding the features of each. Regulatory entities and some membership groups will often facilitate panels with all recognized accreditors to help providers select the accreditor that is best for their agency. Here are some questions you’ll want to ask:
How much does your accreditation process cost?
Ask about application fees, accreditation fees, Site Visit fees (scheduled and unscheduled), and maintenance fees. Is there a fee to purchase the standards? If so, how many copies will you need and how often will updates be published in the future? Make sure to ask about required fees and optional fees. For example, trainings might be required and have associated fees.
What is awarded and how long is it valid?
Each accrediting body will have a different length of accreditation award. This is referred to as an ‘accreditation cycle’, which will let you know how long your award is valid and how often you can expect to go through the accreditation process. Some mandates require a specific award length, in these cases the approved accreditors have worked with your oversight entity to meet this regulatory requirement. It’s important to keep all of this in mind when evaluating cost – how many accreditation cycles will your organization undergo over time (including provisional cycles)?
What is included in the accreditation review?
Will the accreditor require all programs to pursue accreditation, or can you isolate individual programs? Will the administration and management areas of the organization be reviewed? Will every site be visited in the review (important to keep in mind when considering cost!)? Does the approach of the accreditor fit your organizational culture? Does the accreditation cover all of the desired service areas (current and future growth plans)?
We encourage all agencies to look toward future mandates as well. We have often seen additional services mandated, and agencies that utilized an accreditor with a whole-organization approach are most prepared for any mandate that comes their way.
How long does it take?
Most accreditation processes take 12-18 months from deciding to pursue to decision. However, the right time to sign up might vary with each accreditor. For example, some accreditors want to hear from you when you’re ready for your Site Visit within 4-6 months. Other accreditors want you to apply before your self-assessment period so that they can work alongside your organization in preparation for the Site Visit.
How is my organization supported throughout the process?
Are you assigned a point person to work with from the accrediting body? Does the accreditor offer trainings? How and when can you ask questions? Does the accreditor provide templates and other tools to support you? Is there an online management system to assist with managing the process? Though every accreditor provides different tools to support agencies in meeting their mandate, it’s important to assess how much guidance and assistance will help your agency thrive in this process.
What is required to maintain our accreditation status?
Once accredited, what is your responsibility for self-reporting changes at your organization? What is the process when your organization adds a new program or a new site? Are there annual reporting requirements and fees? What is your responsibility when it comes to implementation when standards change?
Seek recommendations
Ask peer organizations
Contact a few peer agencies that are already accredited. Think about the characteristics you should consider when identifying a peer – is it population they serve? Their size? Location? Mission? Ask your peers about their satisfaction with the accreditation process, how they managed the work, and when appropriate, if they’d be willing to be a resource while you pursue accreditation.
Ask internally – staff, board members, and volunteers
Start a discussion about their accreditation experiences and what they liked or disliked about the process. This is also an opportunity to gauge interest to see who would be willing to be part of the accreditation team or even lead the accreditation effort within your organization.
Ask your membership associations
If you belong to an association, ask if they support accreditation. Some associations have relationships with accreditors which might make your organization eligible for a discount when pursuing the process. Some offer technical assistance, and many are willing to facilitate dialogue around accreditation.
Hopefully, this information will assist your organization with mapping out your journey towards seeking accreditation.
Here are some related resources we have available.
- Tips for Creating Effective Workgroups
- What’s the difference between accreditation, licensing and certification?
- Accreditor Comparison
Please feel free to share other resources you’ve found helpful while navigating this topic in the comments below!
I’m going to go out on a limb and say it: Mental Health is IN right now. Everyone from meme accounts to rappers is talking about it, and working on your emotional well-being no longer has the same taboo it once did. In fact, some might go so far as to say that your emotional health is intertwined with your physical health (and those of us in the human services field are probably nodding our heads vigorously at this one). Then it follows to reason that if both aspects of our health are equally important, they deserve equal insurance coverage. But is that what’s happening?
Like most things in the world of behavioral health, the answer is….kind of. In 1996, the Mental Health Parity Act was signed into law. It dictated that the annual or lifetime dollar limits in health insurance coverage be equal to medical and surgical benefits. Did this happen? Short answer, no. Long answer, insurers continued to lead policy and utilized the levers at their disposal to reduce costs and ultimately limit coverage. Employers and insurers began to put a larger emphasis on cost sharing, limits and caps on the number of visits with a care provider or number of days in a hospital were imposed, and benefits didn’t extend to substance use treatment. This led to the 2008 passage of the Mental Health Parity and Addiction Equity Act (MHPEA), which gave advocates hope that further protections were being put in place to ensure equal coverage for behavioral healthcare. So now that it’s 2019, are we actually seeing parity?
MHPAEA 10+ years later
Reflecting on the decade-plus since its passage, what has the MHPEA done for health care coverage? The act has done several important things: it made sure that substance use treatment was included in the parity conversation, it protected mental health and substance use services from being subject to more restrictive cost-sharing and treatment requirements, it ensured equitable coverage for out-of-network treatment, and it gave patients the right to request information regarding medical necessity determinations and reasons for coverage denial. Despite these important steps forward in the battle for parity, implementation hasn’t been easy. Behavioral health providers are seeing 17-20% lower reimbursement rates than their medical counterparts, and the oversight varies wildly from state to state. Advocates such as Angela Kimball from the National Alliance for Mental Illness applaud the Federal law for paving the way for the removal of many of the traditional barriers to mental health treatment, but still feel “much more subtle discriminatory practices” remain an issue.
The “much more discriminatory practices” are what experts refer to as non-quantitative treatment limitations, which includes differences in how plans enact utilization management and define medical necessity, separate deductibles and co-pays for behavioral health services, limited options for in-network behavioral healthcare providers, and lower reimbursement rates. According to the Milliman Research Report on parity laws, this has resulted in decreased reimbursement rates for these provider’s services and approximately 32% of patients going out of network for treatment (in comparison to the 6% of patients that go out of network for their medical services).
Parity at the state level
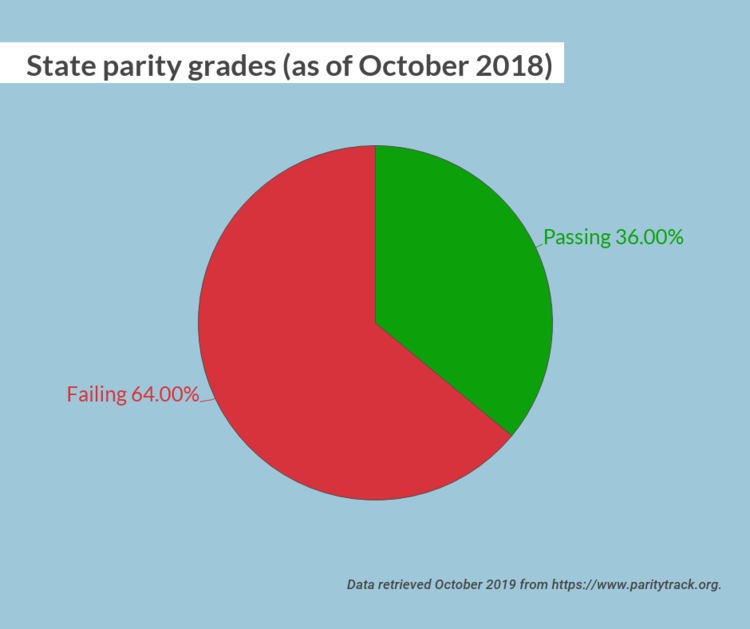
One major road block was inconsistent oversight and implementation at the state level. As recently as October 2018, 32 states received a failing parity grade. However, the state of Illinois was a star pupil, with a 100/100 grade. Illinois went above and beyond Federal parity policy by passing Public Act 99-480, which expands upon the MPHEA with provisions to extend coverage, provide education to the public about their rights, require minimum treatment benefits, and strengthen oversight and enforcement of the law. The Illinois statute extended applicability to plans not covered under the Federal parity law, such as fully insured plans for small employers and state and local governmental plans. It also extended the opioid antagonists covered in the plan. In addition, the legislation required the Illinois Department of Insurance to develop a plan for a consumer education campaign on mental health and addiction parity in order to help consumers, providers, and health plans better understand parity under the law. Finally, the law created an interagency workgroup and clarified the enforcement authority as the Department of Insurance. It’s this last piece, the interagency workgroup and clarification of enforcement, that promises continued success for Illinois parity. It promotes continual work, reflection, and analysis of Illinois’s parity statutes and clear delegation of responsibility.
The state of New York is an example of a state who has struggled with parity implementation but is actively trying to bolster its own Mental Health Parity laws. The Mental Health and Substance Use Disorder Parity Reporting Act was signed into law on December 22, 2018, and creates a reporting mechanism for health plan information to the Department of Finance to increase oversight of behavioral health management companies. The insurers will submit data to the department in order to keep track of potential non-qualitative treatment limitations. This is an important first step to identifying bad insurance coverage policy and protecting consumers.
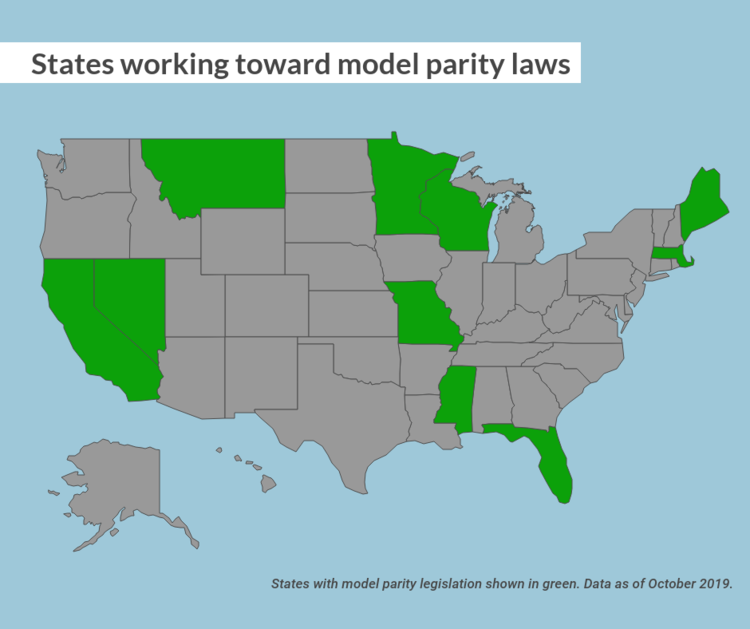
Illinois and New York aren’t the only states who are working towards true parity for behavioral health coverage. Pennsylvania has identified and fined a large insurance company and its subsidiaries for imposed behavioral health treatment, and Wyoming and New Jersey both recently enacted policy for insurers to meet MHPAEA requirements. While the United States might not be at a point where we can safely say we are full parity across the nation, states are taking the steps to get there.
What can I do about health parity?
Glad you asked! For starters, call your legislators! The following states have introduced model parity legislation; contact your state senators and representatives to let them know you want them to support health parity: California, Florida, Maine, Massachusetts, Minnesota, Mississippi, Missouri, Montana, and Nevada.
Don’t see your state here? The American Psychiatric Association has you covered with model parity laws for every state!
At the Federal level, there are several bills that could use your support. Contact your senator or house representative and let them know you support the following bills:
- The Mental Health Parity Compliance Act (S. 1737/H.R. 3165)—This would require comparative analyses about the design and application of managed care practices. That information would then be collected by federal agencies, who would analyze the plans’ compliance, specify what must be done to bring it into compliance, and submit an annual report of their findings.
- Parity Enforcement Act (H.R. 2848)—This bill authorizes the Department of Labor to issue monetary penalties for those violating the federal health parity law.
Reach out to your senators and representatives! Make sure that your state is providing you the best behavioral health coverage possible. Your mental health is just as important as your physical health, and it should be covered. The MHPAEA was an important step in the fight for parity, but we are a decade out from its passage and have learned lessons about the act’s limitations. We should be using those learnings to get us closer to full parity.
