We formally announced today the addition of our fourteenth Sponsoring Organization, the National Council for Behavioral Health (National Council), the unifying voice of America’s health care organizations that deliver mental health and addictions treatment and services.
COA Sponsoring Organizations are separately incorporated, nonprofit national membership bodies comprised of organizations that provide services that are accredited by COA. They share a goal of enhancing the well-being of individuals, families, and communities internationally through the advancement of best practices. Each Sponsoring Organization is represented on COA’s Sponsor Advisory Council (SAC), which advises the chief executive officer (CEO) and provides feedback on COA’s standards and processes.
In addition to having a representative on COA’s Sponsor Advisory Council, members of National Council will receive a 25% discount on their COA accreditation fee.
Jody Levison-Johnson, COA’s President and CEO shared, “I couldn’t be happier about this new partnership with the National Council. The depth and breadth of their knowledge, and their membership will help enhance COA’s ability to advance best practices in behavioral health through accreditation. We are so fortunate to have forged this new collaboration with such a strong leader in the behavioral health field.”
COA and National Council will collaborate on standards development, public policy, and translating trends in the behavioral health field to standards for providing quality services to communities.
“The National Council is thrilled to be a partnering with COA. As a membership organization, our priority is to help behavioral health providers deliver high quality, reliable care to those they serve, and this collaboration will help us further achieve that goal,” said Chuck Ingoglia, National Council’s President & CEO. “Together, we will tackle complex issues and identify vulnerabilities to improve the lives of those we serve.”
About the National Council for Behavioral Health
The National Council for Behavioral Health is the unifying voice of America’s health care organizations that deliver mental health and addictions treatment and services. Together with our 3,326 member organizations serving over 10 million adults, children and families living with mental illnesses and addictions, the National Council is committed to all Americans having access to comprehensive, high-quality care that affords every opportunity for recovery. The National Council introduced Mental Health First Aid USA and more than 2 million Americans have been trained.
Welcome to the Council on Accreditation (COA) blog post series Profiles in Accreditation!
The organizations that COA accredits are diverse in both the communities they serve and their reasons for seeking accreditation (or reaccreditation). Profiles in Accreditation will explore the accreditation experience through the perspective of these organizations. Through them, we can discover the value of accreditation, best practices, lessons learned, and recommendations.
Organization profile
Name: Family Service Association
Location: Lincoln, Nebraska
First accredited: 1998
Latest reaccredition: 2019
Snapshot: Family Service is a nonprofit organization that has been providing services to the families of Lincoln, Nebraska for 125 years. They recently updated their mission to be “Helping Families Thrive.” Currently, Family Service provides families with four programs: Women, Infants, and Children; Child Care Food; Behavioral Health; and Out-of-School Time, which includes before- and after-school care, as well as summer care.
Two of Family Service’s four programs are accredited with COA: Behavioral Health and Out-of-School Time. Their Out-of-School Time program is their largest program. It consists of 14 before- and after-school care programs and seven Community Learning Center programs. Their Behavioral Health program provides licensed therapists to 22 schools within Lincoln Public Schools and six schools in Saunders County. It also includes of a Community Response Program, which connects families with community resources that will support families to meet their goals and strengthen relationships within the community.
Interview with Family Service Lincoln
For this Profiles in Accreditation post, we asked Director of Strategic Initiatives Jessica Radford, Ed.D. to share her experience at an organization that has been accredited by COA for the last ten years. Jessica told us how reaccreditation has helped drive the organization’s quality improvement forward. She also shared how she appreciated how COA accreditation felt not like an evaluation via checklist, but an effort from a team.
COA: What were some of the drivers for seeking reaccreditation this latest time around?
JR: It was important for our organization to seek reaccreditation to learn how quality programs and services are defined and to help us identify areas of growth. All our Management Team was new within the past two years. Reaccreditation provided us with the opportunity to really dig into the organization and its practices. We learned what was done historically, what was currently being done, and how we could improve it.
Accreditation helped us to evaluate and update practices that are oftentimes overlooked. Some of these included safety and risk assessments, HR audits, and an annual review of policies and procedures. It also helped us evaluate our system for communicating with staff and involving stakeholders. Sometimes we forget to evaluate our common organization practices and their effectiveness because we just keep doing things the way they’ve always been done. Accreditation helped us hone in on these practices and improve them.
COA: What about the COA accreditation process made you decide to partner with us?
JR: Our organization has been accredited with COA for the last ten years, and the staff take great pride in this accreditation. COA holds their organizations to high standards and has a rigorous accreditation process. So it was important for Family Service to continue this accreditation with COA for consistency, as well as to ensure we were providing good services to employees and families.
COA:How did you engage and communicate the value of accreditation to the entire organization during the accreditation process?
JR: We held a kick-off meeting where we brought everybody together and talked about the importance of accreditation, the process, and the role they would play. We provided updates through emails and meetings. When we received our accreditation, we had a cookie celebration and invited the board and stakeholders.
COA:What do you see as the main benefit of COA accreditation?
JR: The main benefit for us through our COA accreditation was the framework for evaluating and improving the organization and its practices. Sometimes it can feel overwhelming, not knowing where to begin with improvements or trying to identify what needs to be improved. COA provided a very thorough framework for us to follow, allowing us to assess the organization and its practices comprehensively so that we could target areas to work on. The standards also provided guidance for how to make improvements and what best practices are for nonprofit organizations.
COA: What about the accreditation process do you feel was most valuable to your organization?
JR: All of it. 😊
The standards were easy to understand and provided clear guidance. The staff at COA were very responsive and helpful. They always responded within a day anytime I emailed or called them, and they always had an answer for me. They were also very willing to take the time to help me and make sure I understood the process and standards.
The feedback given to us from our on-site reviewers was also very valuable and appreciated. For example, the on-site reviewers talked with us about the training of the organization. Following this conversation, we purchased an online training system and began implementing it. The system communicates with staff, tracks training completion, and provides lots of training options to staff.
COA: What did you like most about the accreditation process?
JR: I liked all the guidance that was provided through the accreditation process. The standards were very easy to understand and provided lots of explanations through the Interpretations. The staff at COA were so knowledgeable and helpful. The Intensive Accreditation Training was full of great information and guidance. Our on-site reviewers provided lots of great feedback on areas we can improve. The process really felt like a team effort.

COA: What was the biggest challenge during the accreditation process?
JR: Organizing all the evidence. 😊
I found it helpful to organize the standards and evidence into tables. I put together tables with three columns: Standard, Required Evidence, and Family Service Evidence. This helped me to keep track of what document went with what standard and to be sure I provided evidence for each of the areas of Required Evidence. It helped me organize it into more of a checklist.
COA: How has COA reaccreditation impacted operational success?
JR: The reaccreditation has really helped drive our quality improvement forward. It has given us specific areas to improve on and helped us set goals and objectives. It’s only been a few months since we received our accreditation and we have already made some great improvements.
Because of our accreditation, we have worked to improve the training we provide our employees. We have created an onboarding process which includes some safety trainings and some behavior trainings. We have created an annual training plan which includes monthly safety trainings for all staff and bi-monthly supervision trainings for all supervisors. The system we have implemented tracks trainings completed by staff in one on-line system. This has helped us to keep track of trainings as well as identify training needs for staff. This has not only improved our training program, but also the culture at our organization. Staff now feel that safety and training is a priority to Family Service.
We have also become more aware and thoughtful about reviewing our practices on a regular basis. We have implemented annual HR audits, stakeholder meetings and surveys to get feedback on our programs, annual reviews of policies and procedures to make sure they reflect what we are doing, quarterly safety checks and risk assessment reports, and improved data collection to help us analyze practices and programs.

COA: What are the top three pieces of advice or tips that you would give to an organization considering or currently undertaking the accreditation process for the first time?
JR: The coordinator of the process needs to be a very organized person. A large part of the process is collecting and organizing evidence to be submitted. If the person is already good at organizing projects and information, setting deadlines, and delegating duties, this will make the process less overwhelming.
Use your COA team. Do not be afraid to ask questions. Everybody on our COA team was so helpful. It felt more like a team effort instead of an evaluation and checklist.
Use the process as an opportunity to identify areas of growth. Do not try to look perfect for COA. Be honest about your practices and procedures. This will help you use the process to identify areas of growth and make improvements.
COA: Are there any other learnings or insights that you’d like to share?
JR: I cannot say enough good things about our accreditation team. Mary Glenn was amazing, and I couldn’t have done it without her. She was always so helpful and knowledgeable. Even when I felt overwhelmed or like we were doing things wrong, she helped guide me and reassure me that we were on the right track with things.
Our on-site reviewers were so pleasant and knowledgeable as well. They did a wonderful job at the introductory meeting explaining accreditation and the process to our board and staff. All our staff enjoyed having them on site and talking with them. Their feedback during the exit meeting was so valuable as well. It really gave us areas to improve on.
When we received our final accreditation report, nothing was a surprise because everybody had been so transparent through the process. It was really a team effort to get our accreditation, and COA was a big part of that team.
Thank you, Family Service Lincoln!
We would like to thank Jessica for her thoughtful insights into the reaccreditation process, and acknowledge the entire Family Service Lincoln board and team for embracing accreditation and collectively contributing to the promotion of best practices. Thank you, all!
Do you have an accreditation story to tell? Click here to share it. You could be the next organization we feature!
I’m going to go out on a limb and say it: Mental Health is IN right now. Everyone from meme accounts to rappers is talking about it, and working on your emotional well-being no longer has the same taboo it once did. In fact, some might go so far as to say that your emotional health is intertwined with your physical health (and those of us in the human services field are probably nodding our heads vigorously at this one). Then it follows to reason that if both aspects of our health are equally important, they deserve equal insurance coverage. But is that what’s happening?
Like most things in the world of behavioral health, the answer is….kind of. In 1996, the Mental Health Parity Act was signed into law. It dictated that the annual or lifetime dollar limits in health insurance coverage be equal to medical and surgical benefits. Did this happen? Short answer, no. Long answer, insurers continued to lead policy and utilized the levers at their disposal to reduce costs and ultimately limit coverage. Employers and insurers began to put a larger emphasis on cost sharing, limits and caps on the number of visits with a care provider or number of days in a hospital were imposed, and benefits didn’t extend to substance use treatment. This led to the 2008 passage of the Mental Health Parity and Addiction Equity Act (MHPEA), which gave advocates hope that further protections were being put in place to ensure equal coverage for behavioral healthcare. So now that it’s 2019, are we actually seeing parity?
MHPAEA 10+ years later
Reflecting on the decade-plus since its passage, what has the MHPEA done for health care coverage? The act has done several important things: it made sure that substance use treatment was included in the parity conversation, it protected mental health and substance use services from being subject to more restrictive cost-sharing and treatment requirements, it ensured equitable coverage for out-of-network treatment, and it gave patients the right to request information regarding medical necessity determinations and reasons for coverage denial. Despite these important steps forward in the battle for parity, implementation hasn’t been easy. Behavioral health providers are seeing 17-20% lower reimbursement rates than their medical counterparts, and the oversight varies wildly from state to state. Advocates such as Angela Kimball from the National Alliance for Mental Illness applaud the Federal law for paving the way for the removal of many of the traditional barriers to mental health treatment, but still feel “much more subtle discriminatory practices” remain an issue.
The “much more discriminatory practices” are what experts refer to as non-quantitative treatment limitations, which includes differences in how plans enact utilization management and define medical necessity, separate deductibles and co-pays for behavioral health services, limited options for in-network behavioral healthcare providers, and lower reimbursement rates. According to the Milliman Research Report on parity laws, this has resulted in decreased reimbursement rates for these provider’s services and approximately 32% of patients going out of network for treatment (in comparison to the 6% of patients that go out of network for their medical services).
Parity at the state level
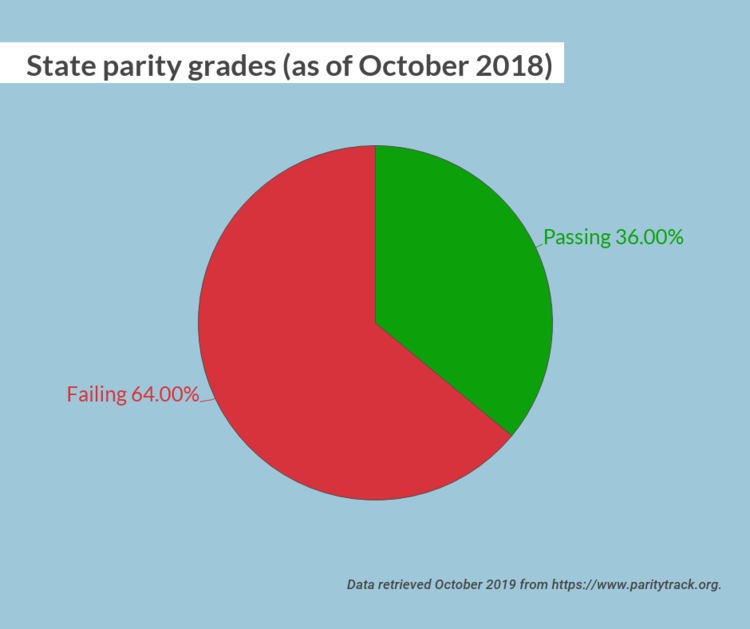
One major road block was inconsistent oversight and implementation at the state level. As recently as October 2018, 32 states received a failing parity grade. However, the state of Illinois was a star pupil, with a 100/100 grade. Illinois went above and beyond Federal parity policy by passing Public Act 99-480, which expands upon the MPHEA with provisions to extend coverage, provide education to the public about their rights, require minimum treatment benefits, and strengthen oversight and enforcement of the law. The Illinois statute extended applicability to plans not covered under the Federal parity law, such as fully insured plans for small employers and state and local governmental plans. It also extended the opioid antagonists covered in the plan. In addition, the legislation required the Illinois Department of Insurance to develop a plan for a consumer education campaign on mental health and addiction parity in order to help consumers, providers, and health plans better understand parity under the law. Finally, the law created an interagency workgroup and clarified the enforcement authority as the Department of Insurance. It’s this last piece, the interagency workgroup and clarification of enforcement, that promises continued success for Illinois parity. It promotes continual work, reflection, and analysis of Illinois’s parity statutes and clear delegation of responsibility.
The state of New York is an example of a state who has struggled with parity implementation but is actively trying to bolster its own Mental Health Parity laws. The Mental Health and Substance Use Disorder Parity Reporting Act was signed into law on December 22, 2018, and creates a reporting mechanism for health plan information to the Department of Finance to increase oversight of behavioral health management companies. The insurers will submit data to the department in order to keep track of potential non-qualitative treatment limitations. This is an important first step to identifying bad insurance coverage policy and protecting consumers.
Illinois and New York aren’t the only states who are working towards true parity for behavioral health coverage. Pennsylvania has identified and fined a large insurance company and its subsidiaries for imposed behavioral health treatment, and Wyoming and New Jersey both recently enacted policy for insurers to meet MHPAEA requirements. While the United States might not be at a point where we can safely say we are full parity across the nation, states are taking the steps to get there.
What can I do about health parity?
Glad you asked! For starters, call your legislators! The following states have introduced model parity legislation; contact your state senators and representatives to let them know you want them to support health parity: California, Florida, Maine, Massachusetts, Minnesota, Mississippi, Missouri, Montana, and Nevada.
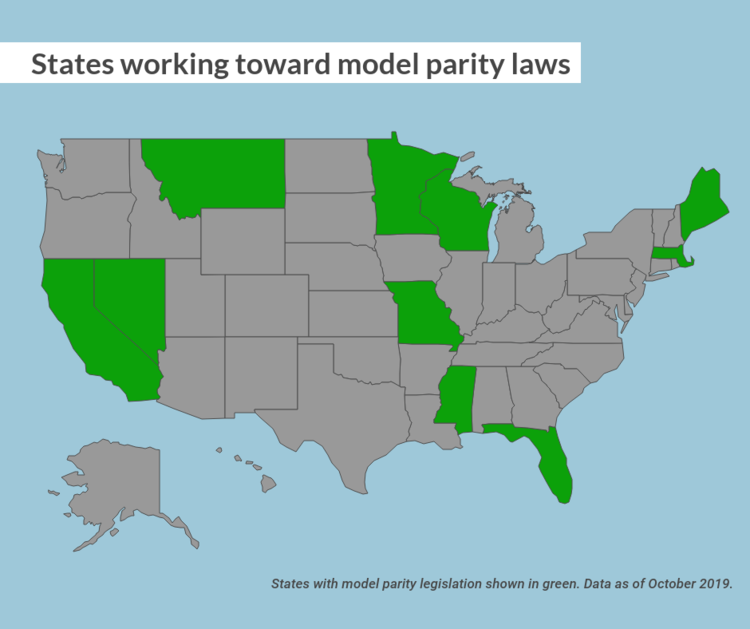
Don’t see your state here? The American Psychiatric Association has you covered with model parity laws for every state!
At the Federal level, there are several bills that could use your support. Contact your senator or house representative and let them know you support the following bills:
- The Mental Health Parity Compliance Act (S. 1737/H.R. 3165)—This would require comparative analyses about the design and application of managed care practices. That information would then be collected by federal agencies, who would analyze the plans’ compliance, specify what must be done to bring it into compliance, and submit an annual report of their findings.
- Parity Enforcement Act (H.R. 2848)—This bill authorizes the Department of Labor to issue monetary penalties for those violating the federal health parity law.
Reach out to your senators and representatives! Make sure that your state is providing you the best behavioral health coverage possible. Your mental health is just as important as your physical health, and it should be covered. The MHPAEA was an important step in the fight for parity, but we are a decade out from its passage and have learned lessons about the act’s limitations. We should be using those learnings to get us closer to full parity.
A big thank you to Tristan Keelan of TenEleven Group for this guest post!
The Behavioral Health field is undergoing a data revolution where electronic capture of daily activity is expected to produce reports that demonstrate, among other things, quality. The initial response to this paradigm shift is to have an electronic health record that can capture data, and produce reporting and analytics capabilities that use the data to demonstrate agency effectiveness. While front-end data capture and back-end information reporting are certainly critical elements of the value based care equation, there is still an element of intervention required by your Quality and Compliance staff to ensure that your data has integrity. To achieve data integrity, you need to make sure that you’re collecting your data in a repeatable manner that provides consistent and accurate data.
Find your outcomes measurement tool
One of the best ways to demonstrate value in behavioral health is to adopt standardized outcomes measurement tools. Tools like the CANS/ANSA, PHQ-9, DLA-20, GAD-7, Columbia Suicide Risk Scale, and many others are designed to allow for the measurement of client populations to be viewed in aggregate for the purposes of demonstrating agency effectiveness. However, the integrity of the outcomes data you capture is going to be critical for framing the story telling that is done once your results are in.
3 tips for maintaining outcomes integrity
The three critical elements that you can manipulate to drive data integrity within your outcomes tools all revolve around creating and enforcing repeatable processes. When your processes are repeatable, you can present your reports with foundational context that improves your presentation. This can turn “here are our numbers,” into “We follow these processes and procedures, which we know drive success, and the proof is here in our numbers.” And the second version is much more convincing.
These three elements are:
1. Determine the cadence that outcomes measures will be captured by, and enforce it.
You want to use standardized outcomes measurement tools so that you can find a way to commonly measure success across your patient population as the progress through treatment over time. Normally when we measure patient outcomes over time, we would make the date the tool was administered the X-axis that would drive our visual; however, in the case of behavioral health outcomes measurement at the agency level we cannot do that.
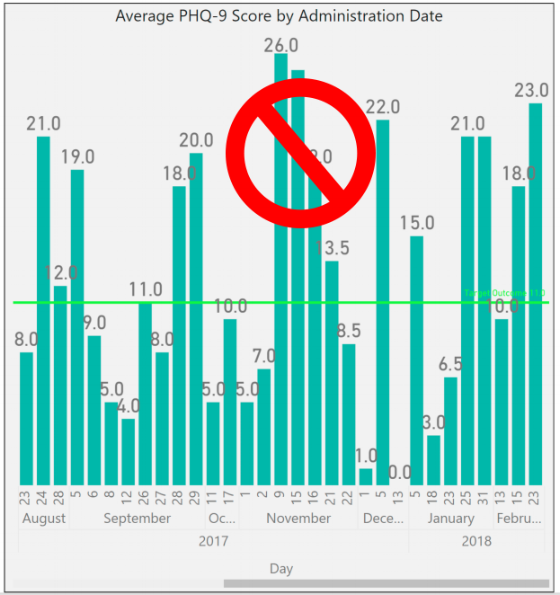
If you were to look at outcomes scores by date, you end up with a mash up of scattered data because clients are not all seen on the same days. For a visual example, look to the PHQ-9 outcomes scores shown in the graph below:
To rectify this and bring your clients into an “apples to apples” view of progress, you must group the scores into the iteration of the form that was administered – first time, second time, third time, etc. When you do that, you bring a focus to what your outcomes look like at the agency level.
The image below shows the same data set, for the same time period, but it is organized with “Administration Number,” as the X-axis to bring the average improvements of client across the agency into focus.
To make this data tell the story you want, you must be able to articulate what your process for capturing the outcomes measurement is. For example, the measure could be administered every time the customer is seen. Or, every 3rd visit. Or, every 3 months (maybe this coincides with treatment plan reviews). Whatever your agency’s choice is, it should be agreed upon, and enforced. From a quality enforcement standpoint, there should be monitoring reports and procedures to follow-up with therapists who have clients fall out of the agency defined outcomes measurement procedures.
Those monitoring reports can also be run historically to determine how often your process is falling outside the desired timeframes, and thus how far off your data integrity is from the desired. If your monitoring reports show that your clinicians are administering the PHQ-9 at different points in treatment for each client, you will have a low data integrity.
Your agency should strive to be able to speak to outcomes in terms of the example phrase, “the positive trend in PHQ-9 scores reflects our process to administer the measurement tool within 14 days of the treatment planning due date, which we achieve 99% of the time.”
When your Behavioral Health agency can add these types of process statements in conjunction with positive trending outcomes reports, then your value proposition appears substantially stronger to your audience.
2. Acknowledge outcome drift – respect the anchors and keep them front and center
Your clinical staff wants their clients to improve; that’s why they got into this business in the first place. However, this presents a common problem for clinical staff who administer scoring tools. Because the desire is for the client to improve, the previous score can often replace the scoring anchors in the subconscious of the person doing the scoring.
For example, consider the following simplistic version of a hypothetical 3 point symptomatic scale.
In the past month, how often did you experience feelings of anxiety?
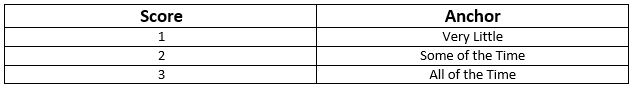
In our example, let’s assume the client has scored a 2 on the past two administrations of the tool. The therapist can begin to rationalize that while the client is exhibiting signs that reflect a 2 = Some of the Time, they seem to be doing better overall. Instead of marking a 2 for the third time in a row on this question, the therapist can begin to use the desire for improvement to justify marking a 1 = Very Little because of the appearance of overall improvement.
This type of “Anchor Drift” is natural and should not prevent the use of standardized outcomes tools, but rather should be protected against. There can be a tendency in EHR software systems to streamline forms in a way that removes unnecessary elements that may have existed in the original paper version. This is where it helps to combat that tendency to drift toward improvement by making the anchors present on the form every time it is completed.
In this case if our anchors, “Very Little,” “Some of the Time,” and “All of the Time” are right next to the questions, it will help to subconsciously override the client’s previous score as the anchor. Stripping out the anchors on an electronic form seems like an efficiency gain of space on the screen, but a smart EHR will keep outcomes anchors present on the form to hold the integrity of the tool above the well-meaning desire for clients to improve.
3. Periodically audit your outcome tool with self-assessments
In conjunction with the previous effort to maintain integrity to the outcomes anchors, you can enforce an audit of your clinical staff compared against your client population. Introduce the client to the outcomes anchors, and ask them and the therapist to each complete separate versions of the form at the same point in the treatment. Then you can measure the variance between them at the agency, therapist, and client levels.
As with all things discussed thus far, there are multiple ways to conduct this audit, and it’s really all about establishing and maintaining process. You can dictate that a self-assessment audit is performed every fourth administration of the outcomes tool. Or, call for random self-assessment auditing at different points and have the audit reflect a date in time, versus a static stage of the process that moves with time. Both methods demonstrate that the agency is committed to maintaining anchor integrity. If the anchor drift feels strong, the agency can move towards refresher training or other follow-up methods that are meant to always keep therapists scoring to the anchors.
Show off your good work
When presenting data, you want to be able to articulate the procedural steps that your agency is taking to ensure that showing a positive trend line can be taken as a representation of actual client improvement. This can make all the difference between winning a contract or being overlooked despite your good work.
The views, information and opinions expressed herein are those of the author; they do not necessarily reflect those of the Council on Accreditation (COA). COA invites guest authors to contribute to the COA blog due to COA’s confidence in their knowledge on the subject matter and their expertise in their chosen field.

Tristan Keelan
Tristan Keelan is the Marketing Strategist at TenEleven Group. Tristan holds a BA in English from Elmira College and an MBA from St. Bonaventure University. He uses his experiences working in Government, Non-profit National Service, and Banking to bring business process and analytics driven insights to the behavioral health industry.
You can read blog posts from Tristan here.
In the high-intensity, resource-scarce universe of human services, the service environment itself often gets overlooked, or else overshadowed by compliance concerns. Against the backdrop of serving families at risk, individuals in crisis, and struggling communities, all while trying to keep the doors open, space planning concerns like layout, furnishings, lighting, and décor can seem trivial. Facility design might sound like a luxury, but in reality it has a presence in almost every aspect of service delivery. The evidence is clear. The physical environment can have a profound impact on behavior, mood, perception, and accessibility. When designed intentionally and strategically, your facility can support the work and mission of the organization. Left unexamined, it can limit or even undercut your impact.
Whether you’re opening a new site, considering a relocation, planning a renovation, or just looking for ways to refresh your facility in a way that improves the effectiveness of your services, here are some important issues to consider:
Safe space
The most fundamental concern for every organization is safety. Every facility has to comply with building codes and regulations aimed at protecting occupants from hazardous conditions. Features like emergency exits are specifically designed to promote safety by influencing behavior in the event of a critical incident – such as evacuating during a fire.
Serving vulnerable populations, however, often means preparing for and responding to critical incidents stemming from distress, conflict, and harmful behavior. In recent years suicide prevention has become a focal point for facility planners and is emerging now as a powerful example of how the built environment can be leveraged to save lives. Organizations serving populations at risk for suicide are embracing the imperative to scrutinize all architectural features, fixtures, and materials in the service environment for their potential to become an instrument for harm – specifically as an anchor point or ligature. Shatterproof glass, round-edged doors and tables, breakaway curtain and closet rods, and tamperproof power outlets are just a few examples of features that have been designed to be suicide-resistant. The layout of the service environment can also play a role in reducing opportunities to self-harm; placing staff areas in close proximity to high-risk individuals allows for consistent yet non-intrusive observation.
A trauma-informed approach tells us that identifying and addressing triggers or trauma reminders is key to preventing and de-escalating crisis situations. Organizations must examine both the physical and psychological safety of their facilities and keep in mind that the built environment itself can be a trigger or stressor. An enclosed, restrictive space can often be triggering for individuals with trauma histories or individuals with certain mental disorders, such as schizophrenia; this is often addressed by foregoing corridor layouts and installing glass doors that enable individuals to get a clear view from one service area into the next. Planners also often avoid using the color red to avoid associations with blood, fire, and emergency lights that can trigger a trauma response. Individuals coping with anxiety or PTSD can be overstimulated by patterns, brightly contrasting colors, or other visually complex designs; neutral or softer colors with more subtle transitions are therefore generally more appropriate for therapeutic environments.
While safety is imperative, there are plenty of other ways the built environment intersects with organizational goals and priorities. Now that we’ve looked at how the physical environment can reduce suicide, harmful behaviors, stress, and aggression, we can turn to how it can reinforce and encourage positive behavior and promote better client outcomes.
The client experience
A well-planned facility should complement your organization’s work by ensuring that individuals and families feel safe, supported, and in control while they are receiving services. To learn more about how organizations use the built environment to support their work, we spoke with Children’s Institute, Inc. (CII) in Los Angeles, a COA-accredited organization that provides a broad array of mental health, early care and education, child welfare, family support, and youth development services to children and families – who are also currently in the process of relocating one of their sites and constructing a new campus.
A client-centered approach informs many of the crucial decisions CII has made in identifying and designing their new facilities. “We thought about how it would affect the client’s experience, being on one floors or two,” says COO/CFO Eugene Straub. CII has been careful to ensure that their facilities are welcoming to both clients and staff. “The goal is building a sense of trust and security. The last thing you want to do is make anyone feel uneasy.” Improvements have also been made to existing sites where the space was not meeting families’ needs. “We had a nice lobby and waiting areas but there were no activities, and we looked for ways to change that and make the space more inviting and inspiring.” Now CII’s once-empty waiting areas include a lending library and creative space for children and families to use.
What are some ways that your organization could find inspiration and ideas when planning facilities? Your service recipients, staff and community are a great resource for ideas and a great place to start. Organizations should always look to their service recipients and their communities for ways to enhance their service environment, and tailor their facilities to the unique needs of the service population and to their service model. For example, a residential facility for individuals with schizophrenia can provide some relief to residents coping with paranoia by orienting beds and desks to face the door. A youth development program for children with autism spectrum disorder, who often struggle with spatial navigation and wayfinding, should consider applying visual cues to transitional spaces. Every organization’s approach to designing an effective and supportive service environment will be unique and depend on their scope, service population, service model, and culture. But there are a few universal design features that facility designers and environmental psychologists agree contribute to a calming, welcoming, and therapeutic service environment:
Nature equals nurture
Studies have consistently shown that access to nature, whether physical or visual, has a calming effect. Treatment facilities often situate themselves in a natural setting for this reason, but any organization can look to existing assets to bring to their full potential, such as a small outdoor space that can be converted into a courtyard or garden, or installing windows to take advantage of a good view. Organizations that are truly limited can still make enhancements by incorporating plant life into the decor and displaying nature and landscape art, which have also been demonstrated to have a positive and calming effect on mood.
Let the sun shine
Sunlight triggers the release of serotonin, which boosts mood and focus. Research also indicates that the ability to identify time of day through observed sunlight is conducive to re-establishing perception and natural thinking while minimizing disorientation. Natural light also makes small spaces appear larger and more open than they are. Organizations should ensure that they’re maximizing and not obstructing their natural light, such as by moving furniture away from the windows, using window coverings that filter rather than block out sunlight, and opening up any doors and windows that would allow natural light to pass through the facility. Transom lights (windows built into the space above a door) and skylights are also examples of architectural features that maximize sunlight while still preserving privacy.
Power to the people
A client-centered and trauma-informed approach to services stresses the importance of giving service recipients opportunities to have a voice in their service plan and at each stage of service delivery. For survivors and individuals coping with past trauma, opportunities to take control and make their own choices are important exercises in self-empowerment and essential steps on the road to recovery. Current best practice regarding residential facilities stipulates that residents should already be encouraged to personalize and decorate their own space. However, when possible, personal choice should also be extended to the environment by giving service recipients the power to customize lighting, temperature, acoustics, or furniture arrangements. To balance flexibility with safety, facility planners often choose furniture that is too heavy to be thrown or used as a weapon, but that can still be moved around and reconfigured, which gives individuals (or groups, in communal settings) autonomy to situate themselves where they feel safest.
No place like home
Experts typically agree that a safe, therapeutic, non-institutional and homelike environment is the best setting for residential treatment. Some strategies that designers employ to make a facility more warm and inviting include using upholstered rather than hard furnishings to invoke a softer, cozier feel, and mixing and matching a cohesive array of furnishings to avoid a uniform, institutional look. Given that “home” is a cultural construct, cultural competency is vital to ensuring that your environment meets the definition of “homelike” for your service population.
Of course, “home” is about more than just furniture — it’s also about people. When designing or evaluating a facility, organizations must consider not only the service recipient, but their support network. Because an engaged and committed support network is one of the most important contributing factors to positive client outcomes, service environments need to promote and facilitate their ongoing involvement. Organizations should be mindful that an imposing service environment can discourage or inhibit the service recipient’s support network, and evaluate whether their facility accommodates and encourages visiting family and friends as well as any collaborating service providers. Is it intimidating for visitors to access or navigate the facility? Are there welcoming spaces for residents to spend time with their visitors, or to have private conversations?
Supporting your staff
Getting your space to work for your service recipients also means ensuring that it works for your workers. As with service recipients, the environment influences workers’ behavior, mood, and functioning – which in turn impact performance and productivity, and your organization’s effectiveness. In human services, an ineffective environment undermines not only your bottom line but your mission.
The human services field also faces significant workforce challenges – namely recruitment, retention, and secondary trauma. Qualified workers are in short supply, in no small part due to poor funding and stigmatization of the service population. Staff shortages and the difficult nature of the work, which often manifests as secondary or vicarious trauma, lead to burnout and to high rates of turnover. Finally, worker turnover negatively affects client outcomes.
These workforce challenges have been at the center of the design and planning process for Children’s Institute, Inc.’s new offices. With the aim of promoting collaboration and “addressing the adverse effects of the work itself”, CII decided to eliminate cubicles in favor of a communal, team-driven open plan layout that will allow staff to support one another, celebrate their successes together, and foster staff resiliency. Straub observed that the cubicle layout often forces staff “to go from meeting with clients to sitting at their desk by themselves” and process their experiences in isolation. The intent of the new layout is to encourage workers to “have more of a shared experience and focus on wellness and self-care both individually and with each other”. The new offices also feature “decompression zones” – calming work-free spaces for staff to recover, including through meditation and yoga, as well as larger common areas, kitchens, and breakrooms. Evolving workplace norms mean that “the younger workforce wants an office space that fosters support and feels less corporate and more collaborative,” Straub explains, making these amenities not just “perks”, but rather, vital resources that will promote staff wellness and strengthen recruitment of valuable staff.
CII is also allocating space for “drop-in” staff – workers from other sites who are out in the field will be able to use nearby CII offices as a landing spot in between client visits. Straub envisions that this increased “cohabitation” will stimulate knowledge and resource-sharing and enhance linkages for families and continue to build the culture of the agency. Emphasizing the importance of “collaborating with the end user,” CII has also been careful to engage staff in the facility planning process, bringing all staff to tour the new space before signing the lease and soliciting feedback about the environment as part of annual employee surveys. Continuous assessment of a new or revamped workspace is not just good quality improvement practice, it also ensures that the organization identifies and addresses any unforeseen effect on employee functioning. For example, in an evaluation study of behavioral health facilities, researchers discovered that staff in a new facility that had been designed to promote client-staff engagement were experiencing greater burnout in response to the increase in client interactions.
Strategic plans to building plans
Creating a safe, effective, and supportive service environment requires the organization to approach the physical environment as part of its mission. It calls for not only commitment and investment, but also a shift in attitude — away from “being happy just to get the space”, as Straub says, and towards leveraging the space to influence how the organization’s operations are experienced and perceived. By tying together their facilities, mission, and strategic plan, CII’s ambitious expansion project received enthusiastic support from its board and funders. Straub sees the new campus as “an opportunity to create organic change” by leveraging the space to build partnerships with the community; plans are already underway to co-locate with other providers and host community taskforces and other grassroots organizing initiatives.
As much as we’d like the primary takeaway here to be “good facility design is not about aesthetics”, it bears noting that a well-designed facility achieves through its appearance two invaluable objectives: firstly, it destigmatizes the organization’s services and service recipients, and secondly, illustrates the depth of the organization’s commitment to the community.
Tell us in the comments: How has your organization used its facilities to support service recipients and staff? What would you change about your current service environment?
Further reading
Building Better Behavioral Health Care Facilities
Rethinking Behavioral Health Center Design
Designing for Post-Traumatic Understanding
6 Behavioral Health Design Trends