If you were to open a newspaper and select an article at random, chances are you would hit a piece on the American opioid crisis. Whether the news is about a pharmaceutical company being taken to court, a Democratic presidential nominee hopeful’s plan to address the climbing overdose rates, or a report on the effectiveness of Heroin Assisted Therapy, opioid news is everywhere. Does all this attention mean we can expect the crisis to abate?
Most likely not. Projections of opioid fatal overdose rates predict a sharp rise in the coming years, with an optimistic peak in 2022 before leveling off. Dr. Donald Burke, a researcher into the American Drug Epidemic, points to the increasing percentage of individuals who first use after exposure to prescriptions and continue to misuse despite the government’s tightening of regulations as evidence for the continual steady rise. He cautions that “the US has experienced four decades of exponentially increasing overdose deaths, so stabilization in the next 2 to 7 years may be more of a hope than a scientific reality.” One of the reasons for this may be that our current approach to targeting the opioid crisis is like targeting the stems of a weed—no matter how much we cut off, if we don’t address the roots, the weed will just keep coming back.
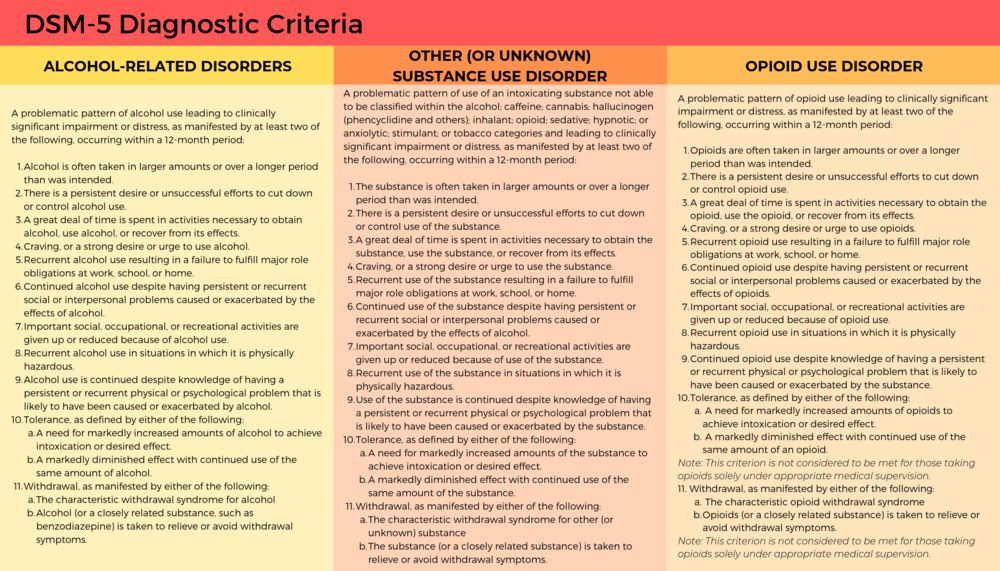
It may be myopic to treat the opioid epidemic as a unique factor in the decreasing American life expectancy. If you look up “Other (or Unknown) Substance Use Disorder” in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) and compare it to opioid use disorders or any other substance use disorder, you will notice the same defining features. So what makes opioids unique? It could be that opioids’ special status comes more from the attention being put on it rather than the drug itself. In the past decade, researchers have found an increase with what they refer to as “deaths of despair”: an overall rise in deaths related to alcohol, illicit drugs in general, and suicide. To address the opioid crisis, we need to look at it in context of these “deaths of despair” and explore its underlying causes.
Substance abuse on the rise
Opioids are not the only drugs that have been on the rise in the last decade. From 2008 to 2013, amphetamine-related hospitalizations increased 245%, and some states have seen the overdose rates surpass those of opioids. Texas is not only seeing a rise in meth use, but also seeing a related increase in rates of life threatening infections, such as HIV and MRSA. In 2015, the state of Wisconsin estimated that meth cost them $424 million, including both the cost of health care and lost productivity. Even opioid overdoses are often not just from opioids: 30% also involve benzodiazepines.
Illicit drugs are not the only culprits when it comes to drastic rises in substance abuse. Between 2002 to 2013, problem drinking rose to the level of a public health crisis, especially among minorities and women, and to unprecedented levels in older adults. According to the CDC, in 2018 over 25% of high school students used a tobacco product in the past 30 days. Beyond the Juul fad that we commonly associate with youth, we have seen a rapid growth of e-cigarette use in adults, with 1/3 of current adult e-cigarette users being those that consider themselves “nonsmokers.”
When you start to look at the numbers it becomes clear: We don’t just have an opioid problem. We have an overall substance abuse problem. This doesn’t even factor in some of the other consumption related disorder (eating, gambling, screen addiction, etc.). Looking at these unhealthy relationships with external stimuli, you can’t help but wonder: What is happening in America to make matters so desperate?
Deaths of despair
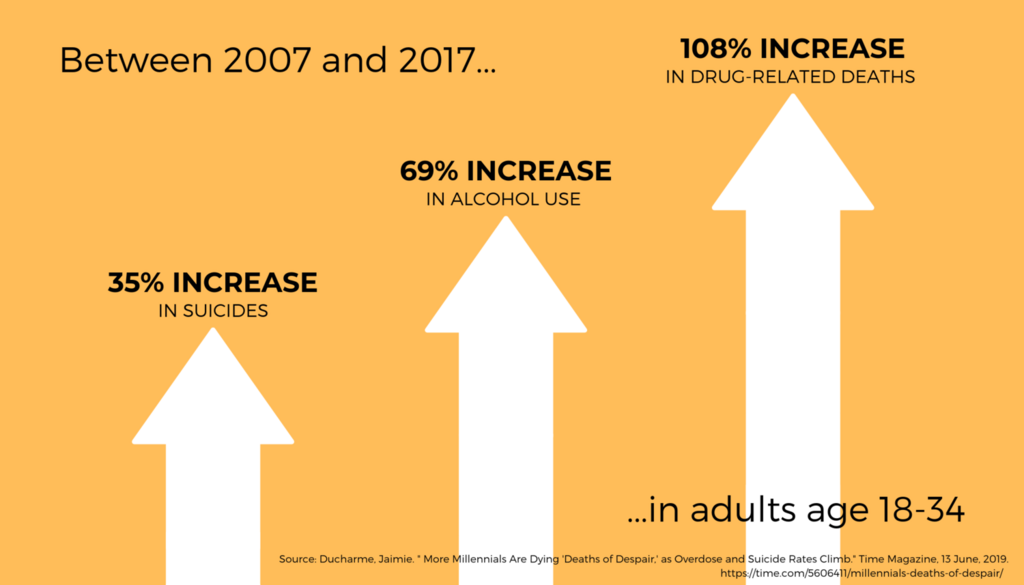
“Deaths of Despair” may sound like a line from an Edgar Allen Poe poem or a new Taking Back Sunday album, but it’s what’s at fault for decline in the average age of American life expectancy. Deaths of despair are commonly agreed upon as those involving drugs, alcohol, or suicide—deaths related to pain, distress, and social dysfunction. Adults between the ages of 18 to 34 have been hit particularly hard–in 2017, 36,000 died from a “death of despair.” For adults between the ages of 45 to 54, the mortality rate rose by a half percent each year from 1993 to 2013. While not as dramatic, that increase has accounted for an alarming decreased life expectancy. If you look at this time period from a societal standpoint, there are a few things that pop out: the Great Recession, the rise of social media, and a rise in loneliness.
While the Great Recession can’t account in its entirety for the current public health crisis, it has played a role. For every 1% increase of unemployment rates, there is a 3.6% increase in opioid-related deaths and 7% increase in emergency room visits, as well as an increased use of tobacco, problem drinking, and other illicit drugs. A comparison of data today versus data from of adults in the mid-1990s and early 2010s shows there have been significant increases of mental and emotional distress, especially among individuals with a lower socioeconomic status.
With increasing rates in social media use, we have begun to see a positive correlation in increasing rates of loneliness. Loneliness has been shown to be positively correlated with suicidal ideation and parasuicide behavior, and a study on young U.S. adults (between ages 19 and 32) found that those with high social media use (around 2+ hours per day) were more than three times as likely to have perceived social isolation, one way that social scientists operationalize loneliness. Studies have shown that conversely, limiting social media use to 30 minutes per day leads to significant improvement in well-being, showing a causal link between the two. Dr. Oscar Ybarra, a professor of psychology at the University of Michigan, theorizes that social media activates social comparisons in users, leading to feelings of inadequacy. While social media can be used effectively as a community builder, it is hard to ignore the relationship between the increased use of social media and the increase of factors that can lead to suicidal thoughts and behaviors, another form of the deaths of despair.
In addition to these factors that cause distress, there has been an increasing sense of loss of community, a protective factor known to mitigate these negative stressors. In his new book, Tribe: On Homecoming and Belonging, Sebastian Junger argues that on our path to modernity, America has paid with the currency of belonging. Much of modernity has been about perfecting the lack of need for others. As people feel increasingly like they can’t measure up to others and have a lower sense of belonging, we’re creating the perfect storm for alienation and depression.
Thinking of substance abuse as a biopsychosocial disorder highlights the relationship between trends in American society and our decreasing life expectancy. This in turn highlights how hard it’s going to be to tackle the opioid epidemic– there’s not going to be one easy solution. The tech sector has responsibility to create community instead of disrupting it, regulators have a responsibility to pass legislation to help get people the necessary supports they need, and we have a responsibility to each other. The opioid epidemic isn’t going to go away any time soon, but we certainly can’t speed up its departure by continuing to ignore the root of the problem.
You are probably familiar with the ripple effect. The term refers to a sequence of events that is triggered by a particular incident or occurrence. The most common example is dropping an object into a body of water…let’s say a stone in a lake. Once it falls, the stone causes a series of waves that spreads across the body of water, the waves ever expanding their reach. The metaphor is often used to describe the potential impact that our actions have on others and the world around us. At times, we may not even be aware of the ripples that we set in motion.
There is no better way to describe the current opioid epidemic. Opioid dependence doesn’t just affect the individual user; it touches the lives of those around them, leaving its mark on children, family members, and friends. And it doesn’t end there. The ripples grow and extend to countless sectors.
One system that is feeling the impact of the opioid epidemic is child welfare. Reports from public officials, advocates, and those working in the field echo the same sentiment – the current crisis is overwhelming. As opioid abuse continues to increase nationwide, the demand for foster care placements is also on the rise. This leads us to wonder what is the relationship, and what does it mean for families and future generations of children?
In recognition of National Foster Care Month, this article will shed light on the connection between the opioid epidemic and child welfare and contribute to the ongoing dialogue on how policy and practice can better support those working with families entrenched in this devastating crisis.
The scope of the problem
Opioid use disorders and fatalities continue to rise
There has been a sharp uptick in the use of opioids since 2010. According to SAMHSA, in 2016, 2.1 million Americans had an opioid use disorder (OUD). As that number continues to rise, so does the number of fatalities. The Centers for Disease Control and Prevention (CDC) reports that 115 Americans die from an opioid overdose every day.
The number of children who have parents struggling with OUDs is unknown. However, a 2017 analysis yielded that 1 in 8 children resided with at least one parent who had a past year substance use disorder (SUD). The report also found that 1 in 35 children lived in a household with at least one parent who had an illicit drug use disorder. Unfortunately, it leads us to consider that parents are among those that we lose to the opioid crisis on a daily basis.
Foster care placements are increasing
Concurrently, as reports of opioid use rise, the demand for foster care placements across the country has also grown. The number of children entering foster care was on a steady decline for more than a decade; however, the tide shifted in 2012. From fiscal years (FY) 2012-16, the number of children in foster care nationally grew by 10%. While individual states varied, more than two-thirds experienced a surge in foster care caseloads during this period. Six states – Alaska, Georgia, Minnesota, Indiana, Montana and New Hampshire – saw foster care populations rise by more than 50%.
More children are residing with grandparents and relative caregivers
Another recent development is the growing number of grandparents taking on the primary caregiver role. Generations United reports that about 2.6 million children – 3.5% of all children nationwide – are being raised by grandparents or relatives across the country. When we look at the data, 32% of children in foster care are being raised by kin, more than previous years. And that may be just the tip of the iceberg. It is estimated that for every child in foster care with relative caregivers, there are 20 children being cared for by grandparents or other family members outside of the foster care system.
Parental substance abuse is a contributing factor for out-of-home placements
What contributes to the need for out-of-home placements? According to the latest national data, parental drug abuse is a factor in roughly one-third of all child removals. While the proportion of children entering foster care due to these circumstances appears to have remained steady over the past few years, it is increasing. Looking across the different categories for removal, drug abuse by a parent had the biggest percentage point growth between FY 2015 (32%) and FY 2016 (34%), which is notable in the face of the current epidemic.
Connecting the dots
So…is there a relationship between the opioid epidemic and child welfare, and if so, what is it? It’s complicated.
Given the timing of these trends, it is hard to imagine that increased opioid use doesn’t play some role in rising foster care caseloads. A recent national study found that counties with higher substance use indicators (drug overdose deaths and drug-related hospitalizations) have higher rates of foster care entry, indicating a relationship between child welfare caseloads and substance use prevalence. However, we have to remember that correlation does not automatically equal causation (proof that what you learn in statistics will come back around) since we can’t control for all demographic and socioeconomic factors and their potential influence on out-of-home placements.
Even though the increase in foster care and relative care placements has been attributed to the opioid epidemic, empirical evidence to prove cause and effect is lacking. This is in part due to the way that the federal government and states track data on child removals, more specifically the contributing factors. For example, there is national-level data on the number of children being removed due in part to parental drug abuse, but it isn’t broken down in a way that shows what type of drug was being abused. Therefore, there is no way to know how many foster care placements stemmed from opioid abuse versus the abuse of another type of illicit drug.
Nonetheless, public officials, advocates and others working in the field are making a direct link between the opioid crisis and increased demand for out-of-home placements. Anecdotally, there are similar accounts across states of the opioid epidemic and its impact on communities. Child welfare agencies are seeing more children come into care because of parental opioid abuse, and children entering the foster care system are getting younger and younger. It has been reported that there aren’t enough foster homes to meet the growing need. Caseworkers are feeling overwhelmed by growing, multifaceted caseloads.
What does this all mean for children and families?
Substance use disorders impact on families
Let’s take a step back. To understand the ripple effect of the opioid epidemic, we have to first look at how parental substance abuse impacts child and family outcomes. At a foundational level, parents struggling with a SUD may not be able to provide for a child’s basic needs (e.g., appropriate supervision or nutrition). Equally troubling, a child can be deprived of emotional support and positive attachment, critical factors in healthy childhood development. Inconsistent parenting inevitability hinders stability in the home. For a child, life can become chaotic and unpredictable, both of which are associated with negative outcomes. That is why parental substance abuse is a known risk factor for child welfare involvement. A 2016 study found that when compared with their peers, children whose parents faced SUD-related issues were three times more likely to experience abuse (physically, sexually, or emotionally) and four times more likely to experience neglect.
Parental substance abuse and child trauma
We know that trauma experienced early in life can adversely impact a child’s development and have long-term health consequences, and parental substance abuse is a one form of childhood trauma (aka an adverse childhood experience or ACE). Often, substance abuse is compounded with other types of adversity, making the severity of potential negative outcomes even worse.
Research shows that history has a way of repeating itself. Children who grow up with complex trauma are more likely to struggle with substance-related issues. One study found that individuals with five or more ACEs were seven to ten times more likely to have issues with illicit drug use. Other explorations into the topic have yielded similar results. There are a host of reasons why people with past trauma experience are more vulnerable to developing a dependence on substance use. While not all children will experience such consequences, the risks to future generations are far too great and warrant immediate intervention. In order to break the cycle, we have to find a way to address the opioid epidemic that is trauma-responsive.
The role of child welfare
The child welfare system is poised to be a catalyst for change. Agencies are tasked with protecting children from maltreatment, abuse, and neglect, and in-home services play a critical role. In-home services are aimed at promoting the well-being of children by ensuring safety, achieving permanency, and strengthening families. When faced with familial challenges, keeping children with their parents is optimal (as long as it is safe and appropriate). Children do best in families with the support of at least one caring adult. Even in crisis, children can thrive when the right protective factors are in place. Removing a child from his or her home disrupts daily life and expectations. All of that instability can be traumatic. The stress that stems from coping with parental loss can have long-lasting effects on a child’s emotional, behavioral, and academic outcomes.
Parental substance abuse has long been an issue for child welfare agencies, one that is now amplified by the recent opioid epidemic. Child welfare agencies across the country are inundated with high caseloads. The complexity of the cases given the unique circumstances and service needs of families battling opioid dependence are adding another layer to an already challenging situation. Not to mention, family stabilization and/or reunification is complicated (contender for understatement of the year). Despite what we know about keeping families together, having children remain with their parents may not be in their best interest due to the impact that substance abuse can have on parenting, making out-of-home placements the safest option. What’s more, reuniting children with their parents can be tricky given ebbs and flows of recovery. The tug-of-war that this creates for caseworkers can be challenging to navigate. So, how do we support those working with families experiencing the crisis firsthand?
Where do we go from here?
Implement what works for families
States and localities are getting creative and implementing interventions that have proven effective for families, recognizing the trauma associated with parental substance abuse. There is ample support for family-centered treatment for substance abuse, including opioid dependence. Additionally, program models that focus on systematic change and cross-system collaboration have also been linked with favorable outcomes.
- Sobriety Treatment and Recovery Teams (START) is an intensive, integrated program for families experiencing co-occurring substance use and child maltreatment. START launched in Cleveland, Ohio in 1997 and extended to Kentucky roughly a decade later. The program matches up specially trained child protective services workers with family mentors (peer support specialists in recovery), behavioral health treatment providers, and the courts. The goals of the program are to ensure child safety and reduce the need for out-of-home care. A 2012 study on the impact of START on family outcomes found that mothers who participated achieved sobriety at a higher rate than those in more traditional treatment programs. Children were also placed in the custody of the state at half the anticipated rate.
- Medication-assisted Treatment (MAT) – an approach that combines medication with counseling and behavioral therapies – is a best practice, and has been linked to decreases in negative outcomes (e.g., opioid use, opioid-related overdose deaths, criminal activity, and infectious disease transmission) and increases in social functioning and retention in treatment, two factors that play heavily into improved parenting skills. MAT has also been found to be effective in providing care for pregnant women who struggle with opioid dependence. Despite some misconceptions in field out the approach, MAT has been associated with improved prenatal care, reduced illicit drug use, and better neonatal outcomes.
- Family Treatment Drug Courts (FTDCs) are specialized courts that respond to cases of abuse and neglect involving caregiver substance misuse. Using a family-friendly approach, FTDCs combine judicial oversight and comprehensive services by bridging together substance use treatment, child welfare services, community supports, and the court system. The unique model balances the rights of both children and parents and aims to create safe family environments while treating the parents’ underlying substance use disorder. In 2015, there were a reported 300 FTDCs across the country, with models and implementation varying state-to-state. The benefits associated with FTDCs include higher participation rates and longer stays in treatment (when compared with non-FTDC participants). The model also yields positive child outcomes; children reportable spend less time in out of home care and are more likely to be reunified with their parent(s).
Support for child welfare agencies and caseworkers
Child welfare agencies are first responders to families in crisis. Caseworkers can encounter stressful or traumatic experiences working with families opioid dependence, witnessing the aftermath of a parental opioid overdose is just one devastating example. That is why supporting frontline staff is imperative.
Provide Specialized Training
Reports indicate that there can be gaps in knowledge among caseworkers around the needs of families with substance use issues and the treatment of opioid use disorders. Training and support in these areas is critical for those working in the field. Additionally, specialized training around recognizing and responding to trauma and trauma-informed care practices is needed when working with families impacted by opioid abuse, as there can be long-lasting negative effects for children if trauma symptoms go undetected and untreated.
Promote Workforce Well-Being
Organizations should employ strategies to reduce secondary trauma and burnout in order to promote workforce well-being. Approaches to reducing the adverse effects of include:
- helping staff identify and manage the difficulties associated with their respective positions;
- encouraging self-care and well-being through policies and communications with personnel;
- offering positive coping skills and stress management training; and
- providing adequate supervision and staff coverage.
Encourage Systems Coordination
Families with substance use issues frequently face other risk factors. Collaboration with other service providers is crucial in helping link parents and their children to the services that they need. The surge in opioid use has trickled into a number of child and family-serving systems. As such, agencies should take steps whenever possible to develop partnerships in their communities to support the work.
Allocate Federal Resources
The crisis is too far-reaching to not have a comprehensive, coordinated federal plan of action in place. Despite declaring a public health emergency, we have yet to devote the level of funds that are needed address opioid dependence. While social service providers and child welfare agencies continue to try and mitigate the impact on a local or state level, the importance of allocating appropriate federal resources to support these efforts cannot be overlooked.
For example, the Maternal, Infant and Early Childhood Home Visiting Program (MIECHV) funds home visiting programs that aim to promote positive parenting practices and healthy parent-child interactions. These programs can also link parents struggling with substance dependence to appropriate treatment providers. Research shows that no matter what level of care is needed, the most beneficial approach is the one that treats families together. MIECHV could help address the unique service needs of the growing number families impacted by opioid dependence.
The Family First Prevention Services Act (FFPSA) may also be a way for federal resources to help child welfare agencies respond to the epidemic. FFPSA is poised to dramatically overhaul the child welfare system, putting federal dollars toward prevention programs and interventions aimed at keeping families together. Substance use treatment programs are among the services that can be prioritized through the restructuring of funds. Additionally, given the increased demand for foster care and relative caregiver placements, advocates are calling to strengthen foster parent recruitment and retention efforts and kinship navigator programs. Increasing capacity in these areas will in turn aid child welfare agencies in finding safe, appropriate placements for children impacted by the current crisis.
There are a variety of other ways that programs and policies could provide relief at a national level; however, equally important is the need for improving data collection across various systems to make informed and evidence-based decisions.
The thing about the ripple effect…
It is hard to stop once it gets put in motion. But that doesn’t mean we shouldn’t try. While the current crisis is overwhelming, there are proposed solutions, ones that can positively impact families and change the course for future generations.
We encourage you to share your thoughts on this important issue. How has the opioid epidemic impacted your community and the children and families you serve? What has been the response? Share your feedback in the comments below!